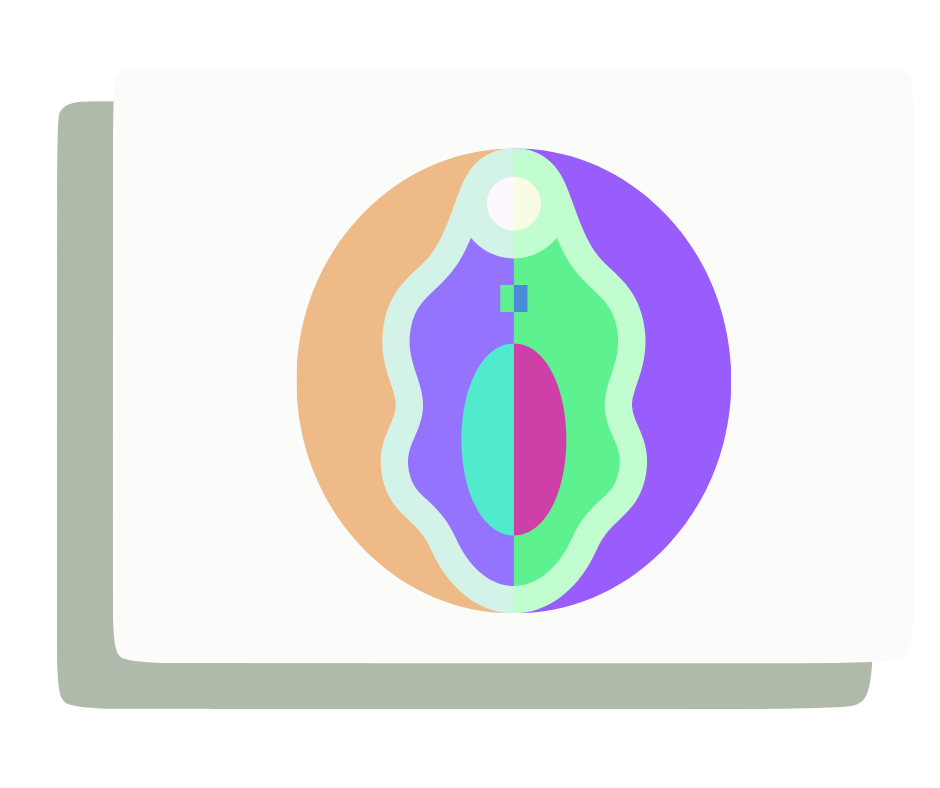
Vulvo-Vaginal Conditions
- Vulvodynia
- Vestibulodynia
- Lichen schlerosis
- Pain with ejaculation
- Bartholin glands inflammation
One of the common vulvo-vaginal conditions that Pelvic physios treat is Vulvodynia or Vestibulodynia- which literally means pain in the vulva or pain in the vestibule respectively. Some common symptoms of Vestibulodynia are:
Common symptoms of Vestibulodynia are:
- Burning sensation in the vulva
- Pain with touch or pressure
- Pain with intercourse
- Pain with tampon insertion
- Pain with gynecological exams
- Redness and swelling of the vestibule
Causes for vestibulodynia can be:
Hormonal:
The vestibule's proper functioning is dependent on both estrogen and testosterone. Any condition that reduces these hormones can potentially cause Vestibulodynia.
Examples: Pain starting after taking combined birth control pills, use of Tamoxifen, Spironolactone, and removal of the ovaries.
Inflammatory:
Chronic infections, severe allergic reactions from substances like toilet paper, bath products, etc. People experiencing this may have "sensitive skin."
Neuroproliferative:
This refers to an increased number of nerve endings, which leads to increased sensitivity in the affected area.
Congenital or acquired:
Persistent infection, recurrent allergic reaction, and persistent inflammation. These conditions can increase the number of nerve fibers in the vestibule.
Overactive Pelvic floor:
May be linked to bladder or bowel symptoms such as urgency/frequency and constipation. When pelvic floor muscles are the cause, the pain is usually limited to the lower part of the vestibule, specifically the 6 O'clock position.
Another common condition is Lichen Sclerosus.
This is an autoimmune skin condition. It causes skin atrophy, hypo-pigmentation (whitening), and scarring. These effects lead to a loss of skin elasticity, making the skin more susceptible to tearing.
Lichen sclerosus can make intercourse painful, as the vigorous force from the activity can cause the atrophic skin to tear. This condition can also result in pelvic floor muscle guarding against the pain, which can eventually develop into a full-blown Pelvic Floor Dysfunction.
Pelvic physical therapy is highlighted as a highly effective adjunct therapy for Lichen Sclerosus to manage pain, reduce tearing by assisting scar remodeling, and decrease pelvic floor tension.
